Our Patients:
Grant and Sebastian Moss

Grant and Sebastian are identical twin boys, who were born to new parents Amber and John on February 27, 2013. Amber had an uneventful pregnancy, and though the boys arrived early at 34 weeks, they came into the world seemingly healthy. After a couple routine days in the NICU stepdown unit of their local birthing hospital, the boys started deteriorating in multiple ways. By day 6 of life, both boys were lethargic and having trouble feeding and breathing. Doctors acted fast to determine why Grant and Sebastian were struggling. Within a 12 hour period, both boys were intubated and their blood ammonia levels were dangerously high. Newborn screens still pending, doctors suspected a genetic cause at the root of their symptoms. A full genetic workup was needed, as well as intensive supportive care. It was quickly decided to transfer Grant and Sebastian to SSM Health Cardinal Glennon Children’s Hospital.
Both boys arrived later that same evening to the Dana Brown Neonatal Intensive Care Unit, courtesy of the SSM Health Cardinal Glennon transport team. “It was all hands on deck,” Amber recalls, reflecting on the vision that unfolded as she approached the boys’ rooms. “I had no idea what was going on. There was so much equipment and so many teams of people. I was told we needed to be at Glennon because of the Genetics specialists here, but at that point, the focus was more just trying to keep them alive.”
Amber recalls one of the nurses pulling her aside upon her arrival. “She was so patient, and so calm. She explained that all these people were collaborating on a plan to get the boys’ ammonia levels down – since that was likely causing their other body systems to fail. All the chief doctors were there – the chief neonatologist, the chief surgeon, the chief kidney doctor, the chief geneticist – all trying to figure out a plan for my boys. Within hours they were both on this combination of dialysis and ECMO,” Amber said.
“The Glennon NICU has rooms especially designed to accommodate twins. The rooms are so large that twins or triplets can usually be in the same room. My boys were on so much equipment that the room wasn’t large enough, so they both had to be in separate twin rooms. Nurses were working extra and moving their schedules just to take care of my babies! Sometimes there were 2-3 nurses working on them at a time; one managing the dialysis; one managing the ECMO, and one doing everything else,” said Amber.
As the next several days unfolded, the boys began to stabilize, Amber grew relationships with the nurses and staff, and she was able to talk more in depth with the Genetics team. “They were putting all the puzzle pieces together,” Amber said. “The boys’ newborn screenings had finally come back, and Dr. Braddock (the Geneticist) was running some more specialized genetic tests with a biochemist he had connections with at SLU.”
Dr. Braddock diagnosed Grant and Sebastian with Propionic Acidemia. Propionic Acidemia is an inherited, rare metabolic disorder characterized by the lack of an enzyme involved in the breakdown of amino acids (the building blocks of proteins). Children who have it are unable to process certain parts of proteins and lipids (fats) properly, which leads to an abnormal buildup of organic acids and toxins in the body. Symptoms typically become apparent in the first weeks of life, and many include diminished muscle tone, poor feeding, vomiting, lethargy, dehydration and seizures. Without appropriate treatment, the accumulation of excessive levels of acids in the blood and body tissues affects nearly all organ systems in a dangerous way.
“Both the babies had been taking breastmilk and formula since they were born – both of which have lots of protein. Their poor bodies couldn’t handle it and weren’t able to break it down. Essentially, that’s what put them into crisis,” said Amber.
Both boys remained in the NICU for over a month. Amber said, “One of the biggest challenges to getting home was feeding. Nutrition is the main form of treatment for them. They have to follow a specific diet their whole lives, including low protein intake, but they have very specific food formulas so their bodies don’t compensate for lack of nutrition.” Amber said, “We were actually really nervous to go home. After all they went through and how critical they were, the boys didn’t go home with any tubes or equipment. But we knew how closely we needed to regulate their food, and how closely we needed to monitor different signs and symptoms. It was really very scary,” she said.
Long term treatment includes a low protein diet in combination with medical formula (medical foods) that are low in certain amino acids. Symptoms of metabolic “trouble” or crisis may include vomiting, lethargy, low muscle tone, failure to grow or gain weight, dehydration or seizures. Amber monitors both boys for these symptoms, and also checks the boys’ urine ketones daily.
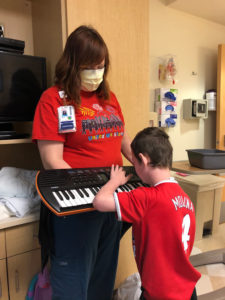
Grant and Sebastian have had several ED visits and re-admissions to the hospital throughout the years. Both boys have port-a-caths for intravenous access and blood draws, and they both have gastric buttons for some of their nutritional needs. During acute episodes, the boys’ treatment might require fluid therapy, measures to provide the appropriate nutritional intake, or administration of certain medications to prevent or treat infection.
Grant had one admission to the hospital which required support of the Pediatric Intensive Care Unit. “He had to be intubated and required a ventilator and dialysis because his lactic acid levels were so high and they wouldn’t come down. Despite all of our efforts to regulate, his levels somehow got really high. It could have been a virus. We don’t really know. Any kind of stress on their bodies, can throw them off balance. He spent a week in the PICU and needed some rehab after that,” Amber recalled.
The constant “stress” on the body from this nutritional balancing act leads to progressive damage over time. As patients age, they can experience various symptoms affecting nearly all organ systems including brain damage, intellectual disability, vision problems, pancreatitis, heart rhythm problems, osteoporosis, chronic renal or heart failure, low blood counts, immune deficiencies and more. Grant and Sebastian have their primary care doctor visits at SSM Health Cardinal Glennon’s Danis Pediatric Center. They are also followed by the hospital’s Complex Care Team, and Footprints, the hospital’s palliative care team. The boys’ care is a coordinated effort involving many specialties including Genetics, Neurology, Nutrition, Immunology, GI and Ophthalmology, just to name what’s current. “Some specialists we now see only annually. Some we see every three months or every six months. Those are the scheduled visits, but we usually land in the hospital for one or both of the boys at least once every month,” says Amber.
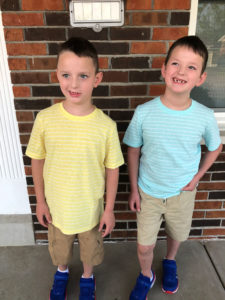
When asked about life outside the hospital, Amber says, “The boys are in second grade, and they have OT, PT and Speech Therapies at school. Both love to cause a decent amount of chaos,” jokes Amber. “Grant loves to have books read to him and to look at books. Sebastian enjoys cleaning and making sure everything is in order. Neither needs to be asked twice if they want to go outside to play. Mickey Mouse is a household favorite of the boys and they don’t miss any chance to spend time with Papa, Maw Maw and Uncle Kyle. My biggest challenge is keeping them healthy and making sure that they are able to live their best lives. I try my best not to let them feel like they have limitations. What the future will look like is really unknown.”
Amber refers to SSM Health Cardinal Glennon as her “home away from home”. “The staff are truly so amazing – from the nurses and doctors to the housekeepers and greeters at the front desk. When a staff member moves on, it’s like grieving a family member! They are my support system – clinically AND emotionally.” She adds, “The opportunity to be an Ambassador for Cardinal Glennon with Children’s Miracle Network is something I’m excited to do. My boys have a very rare condition. This gives me the chance to talk about it, show my appreciation to the hospital, and also show the community and the world what great work is being done here.”
Tribute to past Cardinal Glennon patient, Sebastian Moss
Sebastian was a soul full of pure joy and happiness for every day life. He was full of energy and of course, a decent amount of mischief! Sebastian loved being outside – playing basketball, swimming with his twin brother, and eating at any restaurant with a drive-thru. His favorite places to visit were the St. Louis Zoo – where he loved riding the train and getting a soft pretzel as a treat, and going to Blues games, where he got to see his favorite mascot, Louie! Sebastian also loved visiting the hospital, even when he wasn’t feeling well as he felt it was his home away from home and he loved his Cardinal Glennon family!