Our Patients:
Liam Rhoades

As a scheduler for an obstetrician’s office, Amy Rhoades from Wright City, MO is no stranger to dealing with expecting mothers. In the fall of 2018, Amy found herself walking the journey of pregnancy herself when she learned she was expecting twins with a due date of January 2019. There was a long history of twins within her family, but nothing to alert her that she would have anything but a “normal” pregnancy and delivery.
At her 21-week doctor’s visit, the Maternal-Fetal Medicine physician communicated two concerns to Amy. Amy was having escalating high blood pressure and pre-eclampsia, and one of the twins, Baby Mason, was found to have significant reversed end-diastolic blood flow, or REDF, a condition that causes poor oxygenation of blood flowing from mom to baby through the umbilical cord. In REDF, the oxygen-carbon dioxide exchange is poor, leading to numerous complications for both mom and baby, including respiratory distress, neurodevelopmental impairment and even death.
After that appointment, Amy spent the next month at SSM Health St. Mary’s Hospital, during which time both twins were closely monitored for development and umbilical blood flow. By 24 weeks, however, Mason’s twin, Liam, was also showing signs of REDF and the decision was made to deliver the twins via emergency C-section. Both twins would need to be intubated to help them breathe.
“I remember Cardinal Glennon’s Transport Team being there,” said Amy. “They brought Mason and Liam to me so I could see them and say goodbye, then they immediately took them to Cardinal Glennon in the ambulance.”
The next day, Amy was allowed a pass to come visit her sons in the NICU for a brief two-hour visit. She remembers that day as if it were yesterday, and all of the emotion that was part of it. Mason weighed only 13 oz. and Liam not much more at 1 lb. 1 oz. Both were under bilirubin lights and she was not able to hold them. “I remember sitting down with Dr. Shakir Mohamed,” said Amy. “He was very straightforward and honest with the boys’ father, AJ, and I, telling us that the next 72 hours were crucial for both boys, and that he couldn’t answer if either would make it.”
Two days later, Amy and AJ received a call at St. Mary’s that Mason had experienced a pneumothorax, which causes a collapsed lung. His small size limited available treatment options. AJ and Amy left St. Mary’s and drove to Cardinal Glennon, knowing what heart-wrenching decisions they would soon be faced with.
Amy reflects gratefully on being able to hold Mason before he died. “I had at least 20 minutes with him to hold and snuggle with him after he was taken off the ventilator. I remember him grasping my finger with his hand and looking at me with his eyes open. I knew right then that his purpose was to be Liam’s guardian angel, and that I needed to continue to focus on fighting with Liam,” said Amy.
Six weeks after delivery, Amy returned to work, with Liam remaining in the NICU. “Liam’s father, AJ, is a PTA student in Iowa, so returning to work was tough,” recalls Amy. “But I wanted to make sure I had time off whenever Liam was ready to come home.” When asked what gave her the strength or confidence to do it, Amy was quick to acknowledge her two top factors: Liam’s nurses and support staff, and the NicView cameras.
Amy recalls a few significant primary nurses that earned her trust early on through their communication style, their compassion, and their genuine passion for their work. “They involved me in everything – Liam’s care, Liam’s care planning. They treated Liam as if he was their own, coordinating his outfits every day, and leaving me notes visible through the NicView camera, knowing that I would be checking in non-stop throughout my workday.
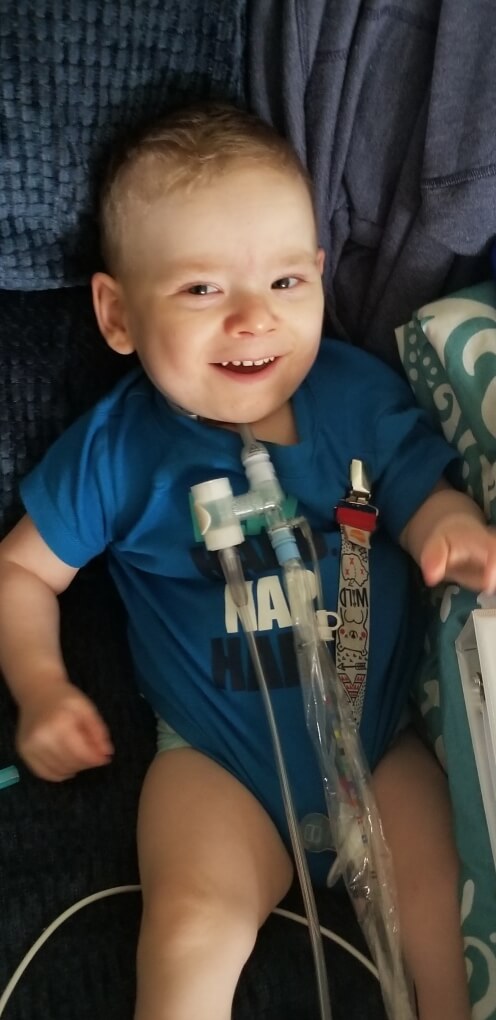
“Liam has had so much happen throughout this whole last year. He had a grade 4 brain bleed soon after birth, hernia repairs, a gastrostomy tube placement for feedings, a ventriculoperitoneal shunt placement due to increased intracranial pressure, frequent transfusions, and so much more! I know we have a ways to go still, but they earned my trust early on,” said Amy.
Liam is living with Bronchopulmonary dysplasia (BPD), a form of chronic lung disease that affects newborns, especially those born prematurely, and infants. It results from damage to the lungs caused by mechanical ventilation respirator and long-term use of oxygen. He had a tracheostomy placed in March 2019, and “graduated” from the NICU to the Transitional Care Unit in September 2019 with a goal to focus on getting home. “It was difficult to leave the NICU environment at first. The staff and the cameras were incredible resources for me as a parent. But the staff on TCU has also become a second family,” emphasizes Amy. When asked to describe some of the support she receives, she was quick to talk about how the Footprints team planned his first birthday party; how the Music Therapist continues to work with Liam; how Liam has already been enrolled into our Complex Care program and STARS program, and how they spent hours helping her feel empowered, teaching her and helping her feel successful at performing all of his clinical care once he is discharged.
Liam is followed by multiple services at the hospital, including (but not limited to) Pulmonology, Neurosurgery, General Surgery, Urology, ENT, Footprints, Occupational Therapy, Speech Therapy, Physical Therapy, Music Therapy, Child Life, and Social Services. He has been on several different ventilators and has finally found the one that will be appropriate for his home use. “The main thing we are waiting for now is home nursing. Liam will need nursing for 16 hours a day,” says Amy.
Despite Liam’s challenges and all of the change and turmoil of this last year, Amy’s perspective is one of positivity and gratitude. “Liam is always smiling and happy. I love watching him enjoy the simple things like his loveys and baby food! I can’t wait to take him outside for the first time and experience all of the ‘firsts’ he has yet to explore,” says Amy. “I have met life-long friends here and formed relationships that have added to my life, and just look forward to getting Liam home and begin our new chapter.”
UPDATE – Spring 2020:
Liam was finally discharged, with a tracheostomy, home ventilator, home tube feedings, multiple therapies and more this past March 2020, during the COVID-19 crisis. He has made great strides since then!
Mom, Amy, shares, “He is almost off oxygen and is only on his ventilator at night! He also got his first haircut!” She adds, “The staff have STILL been amazing, even though we’re not in the hospital! When I call and ask questions they make sure to get me the answers I need no matter what. Thanks for letting us be part of the Glennon family!”
Update – Summer 2024

Liam continues to reach major milestones, including the removal of his trach this past spring! He is starting Kindergarten this fall nearly five years after graduating from the NICU. He has grown from a tiny 1lbs 1oz baby to 42 lbs. and 46 inches tall.
Liam’s mom, Amy shares, “Today at 6 years old, he is living proof that miracles happen at Cardinal Glennon.”