Our Patients:
Zaylen Ball

“The doctors were very nice but straightforward — they told us what the worst outcome could be. If my son had a malignant tumor, he could only have weeks to live,” says Chauncey Ball. “By the grace of God it ended up being just a cyst. It is a blessing.”
His son also was blessed with the recent installation of a new magnetic resonance imaging machine, one of the first of its type, at SSM Health Cardinal Glennon Children’s Hospital.
Zaylen Ball, 4, arrived in the emergency room with headaches, blurred vision and the inability to eat or walk. Doctors in the Dan Dierdorf Emergency and Trauma Center immediately recognized the possibility of a brain tumor and raced him down the hall to the new Imaging Center. The $8.7 million imaging suite at SSM Health Cardinal Glennon was made possible by $6.5 million in contributions to the SSM Health Cardinal Glennon Children’s Foundation.
Preliminary imaging pointed to a dangerous tumor. “A high-grade brain stem glioma is the worst nightmare for any pediatric neuro-oncologist. You have to prepare the family for the worst-case scenario. We tell the family that if it proves to be a high-grade brain stem glioma by imaging, there may be no cure for it,” says Mohamed Abdel-Baki, M.D., a pediatric neuro-oncologist in the Bob Costas Cancer Center at SSM Health Cardinal Glennon and assistant professor of pediatrics at Saint Louis University School of Medicine.
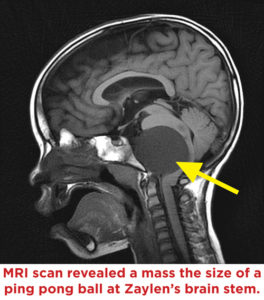
Neuroradiologist Martin Reis, M.D., looks at Zaylen’s images on a bright computer screen in the darkened reading room. He points to an object, about the size of a ping-pong ball, within the base of the skull.
“Initially it was unclear whether the mass arose from the brain stem or was separate from the brain stem. If it was one of the types that is infiltrative, there is a very poor prognosis,” says Reis, assistant professor of radiology at the medical school.
Brain stem tumors are extremely rare and often cannot be removed. The brain stem regulates essential functions such as breathing, heart rate, sleeping, swallowing and coughing. It also contains a bundle of fibers, about an inch thick in a child, holding millions of nerves that conduct messages between the brain’s hemispheres and the spinal cord. Its nerves cannot regenerate if injured.
“His symptoms were typical for a brain stem compression. This looked like a brain stem tumor which is typically inoperable,” says Samer K. Elbabaa, M.D., FAANS, FACS. He is director of the division of pediatric neurosurgery at SSM Health Cardinal Glennon and associate professor of neurosurgery at Saint Louis University.
“DIPG is a diagnosis that we had to consider,” Abdel-Baki says. “It is a tumor that is lethal – Diffuse Intrinsic Pontine Glioma. Only a handful of children have ever been reported to live more than two years with DIPG.” Due to the likelihood of brainstem injury, as standard practice a DIPG is not even biopsied.
About 3,000 pediatric brain tumors are diagnosed in the United States each year, a rate of 3.3 for every 100,000 children. DIPG accounts for 10 to 15 percent of pediatric brain tumors with 300 reported annually across North America and Europe.
Elbabaa and Abdel-Baki joined Reis at his computer screen. Zaylen’s images were compared to views of confirmed DIPG tumors from an online database. There were subtle differences and Zaylen’s symptoms had begun six months previously, indicating a mass growing more slowly than a DIPG.
“It didn’t look like the typical DIPG,” Abdel-Baki agrees.
“Was this a tumor in the brain stem or a tumor in front of the brain stem?” Elbabaa asks.
“Dr. Elbabaa was astute enough to ask us to perform tractography, which can be done much more robustly with the 3.0T MRI scanner,” Reis says.
Eleven months before Zaylen’s admission, SSM Health Cardinal Glennon turned on the latest advance in imaging, a General Electric 3.0T MRI, which holds a magnet rated at three Teslas, the unit of measurement for magnet strength.
The 3.0T MRI succeeds 1.5T machines as the leading edge of imaging and is one of the first in the region and among the first in any pediatric hospital.
MRI (magnetic resonance imaging) produces wonderfully-detailed, three-dimensional images of body structures without utilizing X-ray radiation. The 3.0T machine joined the center’s 1.5T MRI, which remains in service to enhance patient scheduling flexibility. “With higher magnet strength there is more signal, so image quality generally will be superior,” Reis says. “It will improve diagnostic accuracy.” In diagnosing Zaylen’s mass, the heightened image resolution obtained from the 3.0T MRI was enhanced through diffusion tensor imaging.
“The brain is filled with water that moves in a specific direction along axons,” Reis says. “Diffusion tensor tractography follows the movement of water molecules along the axons and gives us a map in three dimensions.”
When Zaylen’s images were processed through tractography, the results vividly showed brain stem fibers curving around the mass rather than going through it. “That made an infiltrating brainstem glioma highly unlikely,” Reis says. “This was something that was potentially treatable.”
Using MRI images and a computerized surgical navigation system, Elbabaa planned a precise surgical journey to Zaylen’s brain stem. Entering through an incision near the base of the skull and behind the ear, Elbabaa reached the mass without touching brain tissue.
“In front of the brain stem we found this very large mass,” Elbabaa says.
“It was a cyst with a thick gelatinous material in it. It was very stuck to the brain stem so it took 10 hours under the microscope to dissect it safely and keep all the nerves and muscles intact.”
The mass was biopsied and identified as a neurenteric cyst, which accounts for about one percent of spinal cord tumors. “That is a benign cyst,” Elbabaa says. “We achieved a cure without the need for chemotherapy or radiation.”
Before the surgery Elbabaa cautioned Zaylen’s parents that he might require breathing and feeding tubes after the surgery. “He ended up without them,” Elbabaa says. “His recovery went much more smoothly than I expected.”
In the weeks following surgery, Zaylen’s brain stem returned to its natural position. He spent nearly two months at the Ranken Jordan Pediatric Bridge Hospital for therapy, recovering abilities that had been hampered by brain stem compression. He sped ahead of expectations and now spends his days shadowing his mother around the house, playing with his cars and video games.
“It is amazing how this turned out. We went from talking to the family about a child that would be dying to a child that will go to college,” Abdel-Baki says.
“He is a normal child who has the potential of a normal 70 to 80-year life expectancy,” Elbabaa says.
Months after Zaylen’s surgery his mother, Zena Townsen, expresses continued amazement.
“I am so blessed. I thought I was going to bury my 4-year-old son. Now I watch him running around,” she says. “I can imagine him turning 16, talking back to me and getting a driver’s license!”
Zaylen and his family spent nearly two months at SSM Health Cardinal Glennon. “Everyone here is so good,” Zena says. They comfort you when you cry. People in the chapel pray with you. You can tell the nurses care about you – they are not just here to do a job.”
Zaylen continues to receive outpatient therapy for speech and for correction of a slight hitch in his walking gait. He is bright, talks constantly and asks questions about everything. He has a special knack for games on fancy cell phones. His grandfather, Herbert Townsen, recently bought a new phone. “I am still trying to figure it out. Zaylen can already get into it. I asked him, ‘Where did you get that information?’”
Other advances in technology – such as imaging – have transformed medicine and surgery within the careers of Zaylen’s doctors.
“Theoretically we could have done this case on the old MRI, but I do think the image quality for things such as tractography is higher on the 3.0T,” Reis says. “Without that equipment, this outcome would not have been possible.”
“The way we do brain tumor surgery now, compared to 10 years ago, is very different,” Elbabaa says. “With the advancements in MRI and other modalities of radiology, we can make surgery minimally-invasive and safer, with less destruction to normal brain tissue. We were thoughtful and careful and had a team approach. That and the technology enabled me to understand this tumor extremely well. I went into the operation having a very meticulous plan for how I would reach the tumor. It helped me be more aggressive.”
The child-friendly imaging suite at SSM Health Cardinal Glennon celebrated its opening on Jan. 24, 2013. In addition to the 1.5T and 3.0T MRI machines, the suite holds two computed tomography (CAT or CT) scanners that create advanced images with lower doses of radiation than previously possible. They can produce brain scans with six to eight times less radiation than the national average.
CT scans produce three-dimensional images based on X-rays and require more radiation than a single radiograph, but new technology has drastically reduced radiation exposure.
“I read recently that a CT scan of the chest 15 years ago was equal to 100 chest X-rays,” says Nathan Bennett, team leader for imaging. “We are doing chest CT at about half a millisievert, which is equal to one or two abdomen X-rays. There is a balance – we can reduce the dose so much that we start to lose image quality. Our radiologists and practitioners are collaborating to get the images they need at doses that have not been seen before.”
Thanks to distractions such as mood lighting and flat-screen televisions showing cartoons, fewer patients require sedation during imaging procedures, Bennett says.
The suite also contains an MRI enhancement that produces images of the beating heart. “Babies have hearts that are the size of a quarter or dime and we are taking pictures of arteries and valves that we were not capable of doing years ago,” Bennett says. “There are maybe five or 10 hospitals in the country doing that.”
With additional equipment has come better service, he adds. “We are able to take more patients and turn the exams over more quickly. We are seeing increased quality, higher service levels and better outcomes.”
SSM Health Cardinal Glennon is one of a handful of pediatric hospitals that contains so much imaging capability, Bennett says, as most use the services of an adjacent adult hospital.
Planning has begun to further expand into empty shell space with four ultrasound rooms, a bone density room, a fluoroscopy suite and three X-ray rooms, one of them a hybrid suite to handle procedures combining surgery and interventional cardiology.